Computing Faculty Supporting Research That Could Cut Cancer Deaths in Half
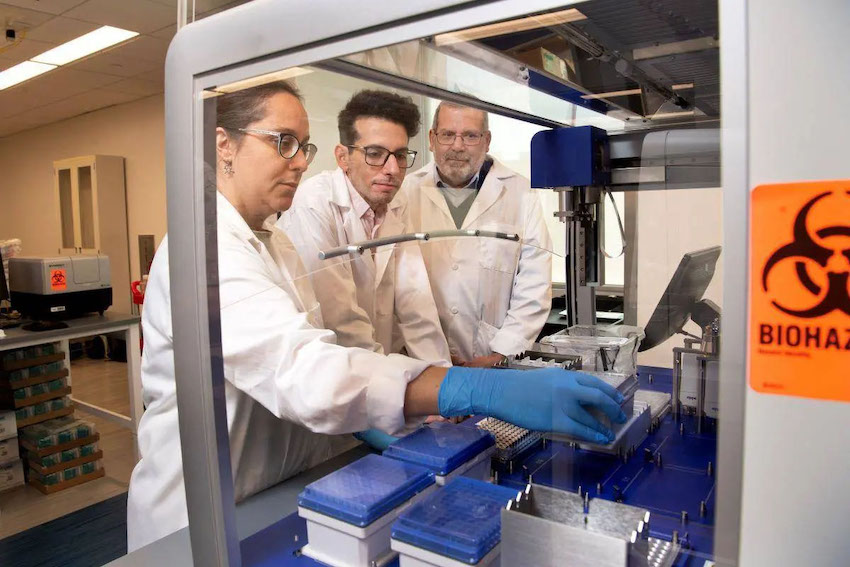
A surgically implantable device the size of a pinky finger could be a huge step toward a cure for cancer. A multi-institutional team of researchers that includes Georgia Tech faculty received $45 million from the Advanced Research Projects Agency for Health (ARPA-H) to develop sense-and-respond implant technology for cancer treatment.
The National Cancer Institute estimates more than 600,000 people will die of cancer in the U.S. in 2023, but the researchers say their project could reduce the number of U.S. cancer-related deaths by 50%.
Josiah Hester, an associate professor in Georgia Tech’s School of Interactive Computing, is a co-principal investigator on the project and is responsible for the sensing and computing technology in the implantable device. He will also assist with large-scale experimentations and coordinate the integration of the technology.
Hester specializes in developing sensing, battery-free, and sustainable technology for wearable and mobile devices. He previously worked on a team that developed the first battery-free handheld gaming console.
Celine Lin, associate professor in Georgia Tech’s School of Computer Science, is working with Hester to develop ultra-energy-efficient chips for signal processing and embedded control. Together, they will develop a robust platform that is energy-efficient enough to last for months.
The device contains genetically engineered cells catered to each individual patient that attack and eliminate cancer cells in the body. Thanks to Hester’s efforts, the device can monitor a patient’s cancer and adjust the dosage of the genetically engineered cells in real time.
“We must keep the cells alive to fight the cancer, and we must understand and control our progress in delivering this treatment,” Hester said. “Releasing too many cells could be toxic, and not releasing enough could be ineffective.”
Omid Veiseh, a bioengineer at Rice University, serves as principal investigator on the project and genetically engineers the cancer-attacking cells.

Along with Hester and Lin, Veiseh’s team consists of 19 co-PIs from the University of Texas, Stanford University, Carnegie Mellon University, Northwestern University, the University of Houston, and Johns Hopkins University.
The researchers named their project Targeted Hybrid Oncotherapeutic Regulation (THOR) and named the implantable device Hybrid Advanced Molecular Manufacturing Regulator (HAMMR).
Over the next five years, the team will test this unique approach to cancer treatment on patients with ovarian, pancreatic, and other difficult-to-treat cancers. They expect to not only improve immunotherapy outcomes for patients, but to make treatment more accessible.
Hester said once the device is surgically implanted, it is designed to remain in the body for six months or more, making it a minimally invasive alternative to chemotherapy.
“If you’re a patient with advanced stage cancer, you might be going in weekly to do various invasive and painful procedures,” Hester said. “This implant could remove a lot of the burden and make cancer treatment more accessible.
“Instead of driving three or four hours to get your treatment — which is expensive, and you may not be able to do it — you can have this implant. You come for the surgery, then you leave, and it stays with you for six months. The localized treatment should reduce the pain and terrible symptoms that chemotherapy and other systemic treatments cause in current protocols.”
ARPA-H is a federal funding agency established in 2022 to support research that has “the potential to transform entire areas of medicine and health.” THOR is the second program to receive funding from ARPA-H after its first Open Broad Agency Announcement solicitation for research proposals.
The first funding contract went to a team of researchers led by Philip Santangelo, a professor in the Wallace H. Coulter Department of Biomedical Engineering at Georgia Tech and Emory. Their project, known as CUREIT, uses mRNA drugs to activate or switch off certain genes to help the immune system fight cancer and other chronic diseases.